How to Tell if Someone Needs CPR

Cardiopulmonary resuscitation (CPR) is a life-saving practice that involves the combination of chest compressions and rescue breathing.
If a person has stopped breathing or blood is not adequately being circulated throughout his or her body, administering CPR quickly and correctly can help to restore circulation of blood to the brain and other vital organs.
The fact is, just a few short minutes without adequate flow of oxygenated blood can lead to brain damage or worse. As such, CPR should be performed as soon as there are signs of a problem.
There are a wide variety of reasons why someone may need to administer CPR.
For instance, when a person has suffered from near drowning, electrocution, smoke inhalation, blunt trauma, drug overdose or an obstructed airway, just to name a few. Regardless of cause, however, the indications that CPR is needed are pretty much the same across the board.
And knowing what to look for is of the utmost importance.
One thing to note: it’s strongly advised that before assessing someone for whether they may require CPR, you should first determine whether the scene itself is safe.
Look around for anyone or anything nearby that could potentially cause additional harm, either to the injured person or to you.
For instance, a room with poisonous fumes, an area where there are downed power lines or the active scene of a crime.
Keep in mind that you won’t be able to effectively assist if you become injured as well.
Even if you do deem the scene safe, you should remain aware of any changes to that status as you render care.
Now, let’s take a look at the recommended steps for determining whether a person needs CPR.
Verify Responsiveness
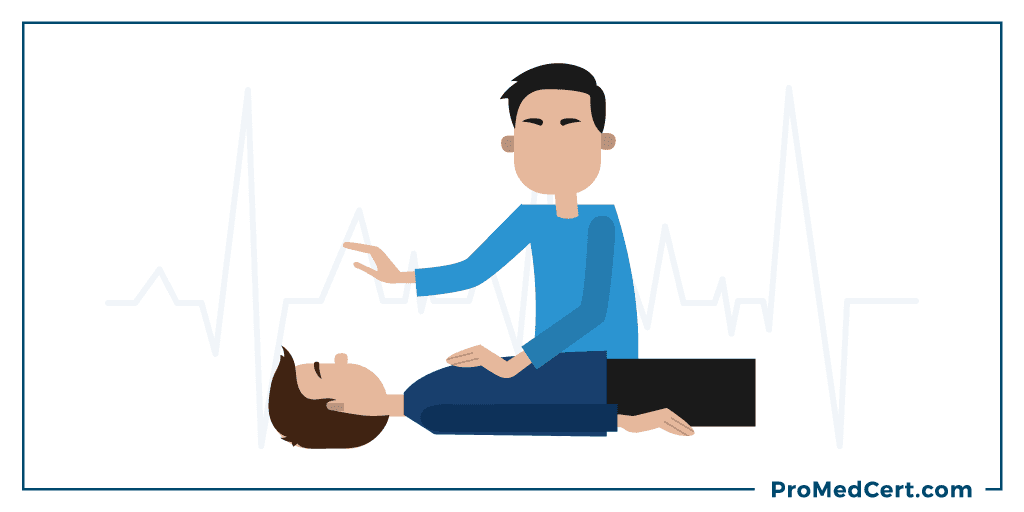
The first step to figuring out if someone needs CPR is to assess their level of responsiveness.
A completely unresponsive individual is unconscious.
This state of being could be caused by some type of injury or simply the lack of oxygen-rich blood flow to the brain.
An unresponsive person may look as though he or she is sleeping.
To determine responsiveness in an adult or child, begin by tapping the shoulders.
If the victim is an infant, determining responsiveness is typically done by tapping the bottom of the feet.
First, approach the individual in question, leaning over or kneeling at his or her side.
Then, tap the shoulders and ask if he or she is alright. (Again, in the case of an infant, tap the feet.)
If the person does not respond in any way by blinking, moving, speaking, crying or eliciting any other action when he or she is tapped, you can confidently deem them to be unresponsive and move on to the next step in the assessment process.
Check for Breathing
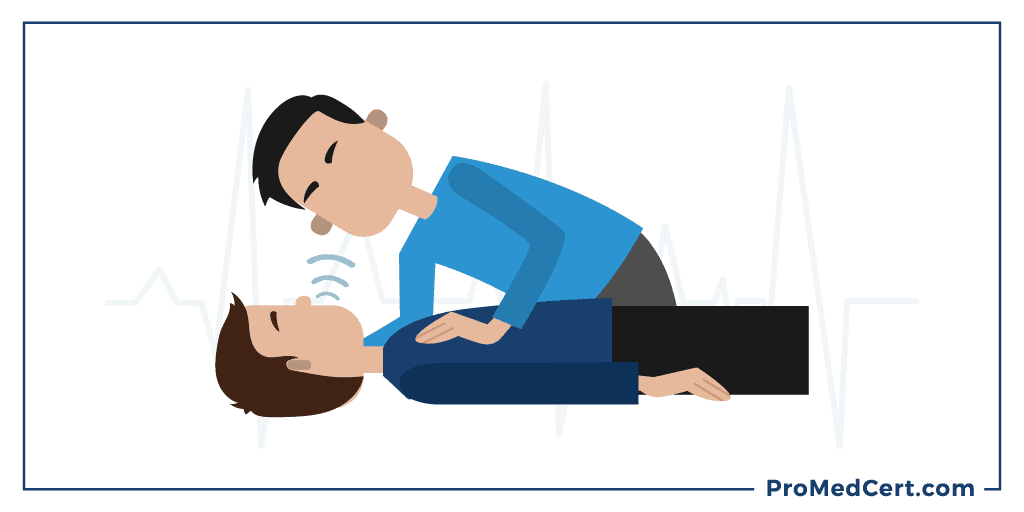
When a person isn’t breathing, he or she isn’t able to adequately take air into his or her lungs.
If someone is breathing, but not normally (i.e. agonal gasps), it could be a sign of cardiac arrest.
These types of gasps are often seen during the first few minutes following the arrest.
Someone who is gasping may look as though he or she is drawing in air quickly,
forcefully and/or weakly.
Moments may pass in between gasps as a result of the slow rate of breathing.
The gasps may sound like a snore, groan or snort.
An individual who is not breathing normally may be more viable than someone who has
stopped breathing completely, but the possibility for brain damage and other serious
bodily injury is still highly likely, so CPR must be started as quickly as possible.
It’s important to point this out, because agonal gasps are frequently mistaken for
live respirations, which can delay the initiation of CPR and result in preventable
harm to the victim.
When a person is experiencing cardiac arrest, in addition to gasping, they may
appear to also have seizures. This is associated with the ventricular fibrillation (V-Fib).
This appearance has also been known to confuse bystanders, thereby delaying the
initiation of CPR.
To assess a person’s breathing status, lean over or kneel at his or her side.
Then, carefully scan the chest from head to waist for a timeframe of at least 5
seconds but no longer than 10.
During this time you should be looking for whether the chest is rising and falling.
If you determine that the person is either not breathing or not breathing normally,
it’s time to start performing CPR.
To improve the odds of success:
Make sure the individual is lying on his or her back on a firm, flat surface
Expose the chest
Initiate CPR beginning with chest compressions
Check for a Pulse
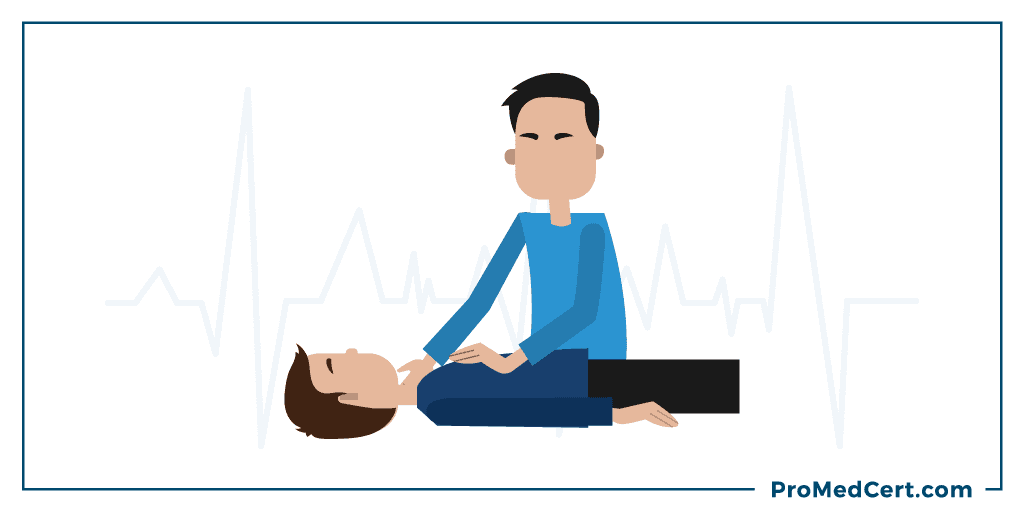
The absence of a pulse indicates that the heart is not actively pumping blood through the veins and arteries.
The best area to check for a pulse on both adults and children is the carotid artery, which is located along either side of the front of the neck, just below the angle of the jaw.
On an infant, the best pulse site is the brachial artery, which can be located by feeling the bicep tendons in the area of the antecubital fossa.
To accurately assess someone’s pulse, lean over them or kneel at their side.
Feel for a pulse on either the carotid or brachial artery for a timeframe of at least 5 seconds but no longer than 10.
If you cannot feel a pulse or you are unsure whether a viable pulse exists, it’s time to start administering CPR.
Again, be sure the person is lying flat on a firm surface, expose the chest and initiate CPR beginning with chest compressions.
Regardless of where you fall in your training (skilled and ready, skilled but rusty or untrained altogether), the way in which you respond in an emergency medical situation can literally mean the difference between life and death.
Conclusion
If a person is unresponsive, is gasping for air or not breathing at all, or does not have a pulse, CPR should be administered as quickly and properly as possible.
Did you know you can become CPR certified for as little as $35?
Click Here to learn more or to sign up for our fast, convenient online first aid certification course.

