The Basic Guide to ACLS ECG Interpretation

ECG interpretation is a critical component in emergency life-saving procedures. It has become an art form of sorts over the years where many medical professionals have invested thousands of hours memorizing and decoding ACLS heart rhythms and their meanings.
The heart is a complex muscular organ, and understanding the basics of how to read ACLS rhythm strips can better equip any medical professional and increase their odds of saving a life.
So, if you’re studying for your ACLS or PALS certification or only want to learn ACLS ECG rhythm interpretation, this guide will help you. Start reading to lay the foundation for interpreting the most common heart indicators you can utilize in real-world situations.
What Is An ECG?
ECG stands for Electrocardiography (sometimes referred to as EKG). ECG and ACLS heart rhythms allow you to see the waves of electrical activity in the heart.
The heart has a normal electrical rhythm. When this rhythm is disrupted, cardiac issues can result. By understanding a normal electrical rhythm vs. an abnormal rhythm, you may be able to quickly diagnose the issue and act to reverse it.
How Is It Helpful For ACLS Or PALS?
ECG Interpretation is very helpful for taking the ACLS or PALS course because understanding an ACLS heart rhythm and recognizing abnormal electrical activity can help diagnose issues quickly.
It can also dictate what responsive procedures are necessary for managing and treating conditions like tachycardia.
A Peak Behind The ECG
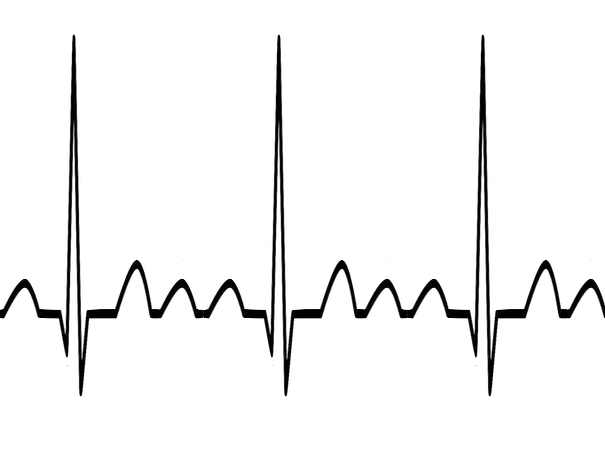
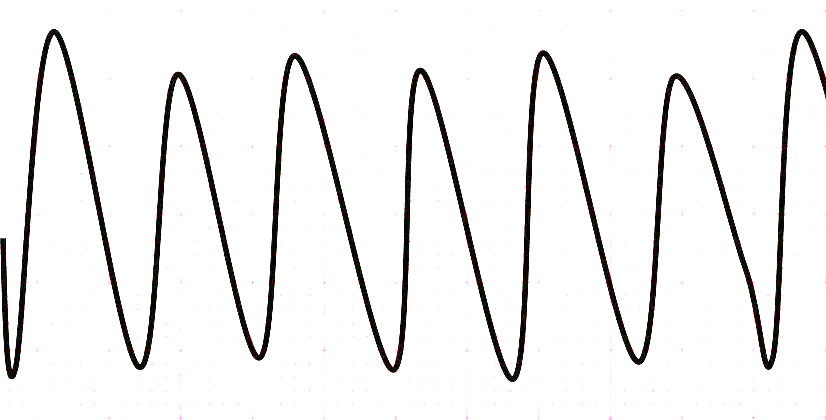
Here’s what a normal ECG strip may look like:
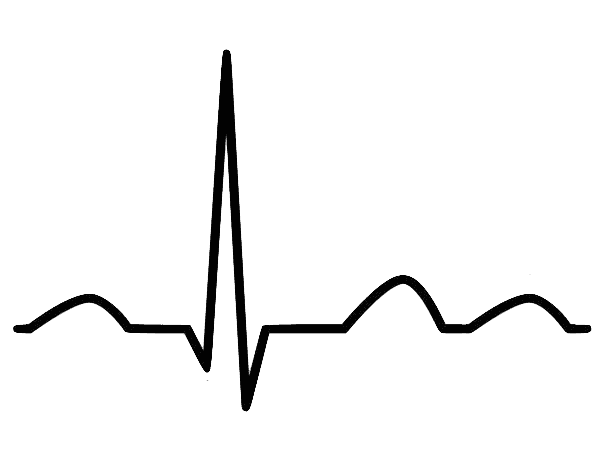
Think of it like this. The above image is a snapshot of what’s happening in the heart. All these dips and waves represent something. For ACLS ECG rhythm interpretation, they each represent a piece of the heart.
To understand this further, let’s explore the basic anatomy of a heart.
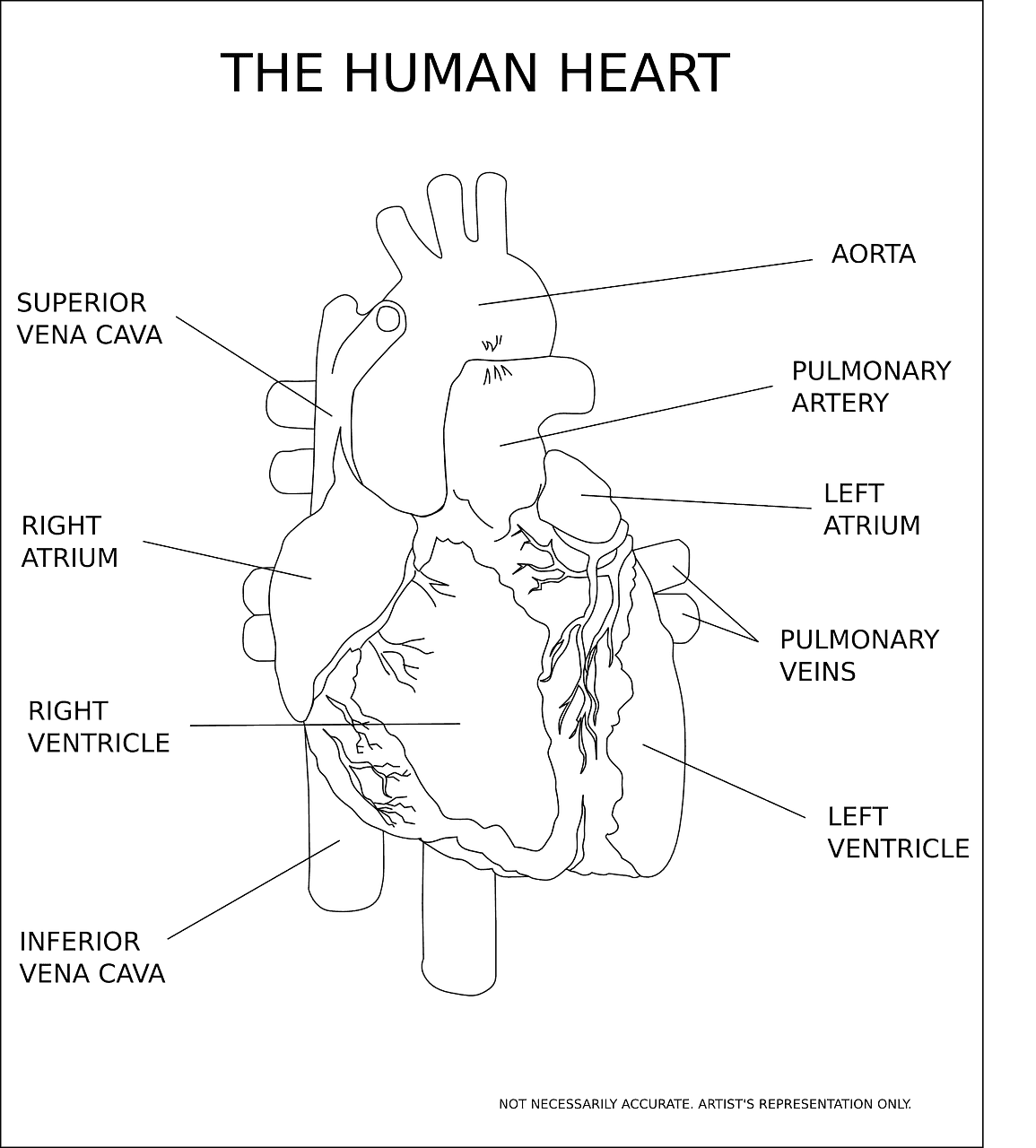
To understand ACLS heart rhythms, you must first understand the heart.
The heart has 4 chambers. The top 2 chambers are referred to as the atriums, and the bottom 2 are the ventricles. Blood enters the heart through the top atriums. Afterward, it's pumped into the ventricles and the rest of the body.
To learn how to read ACLS rhythm strips correctly, you must know that the electrical activity of the heart, controlling this pumping action, is vital in ensuring blood is pumped adequately throughout the body.
Now let’s imagine a beating heart to comprehend how ACLS heart rhythms work:
For blood to enter and exit each chamber of the heart, it has to empty and fill over and over.
This form of blood movement requires a “squeezing” and “relaxing” effect in each chamber you will encounter in ACLS ECG rhythm interpretation. This is controlled by the heart's electrical system.
The electrical conduction system in the heart is made up of:
- The SA Node. This node is located in the right atrium and sets a normal heart rate of 60 to 100 beats per minute.
- The AV Node. This is located in the interatrial septum and sets a rate of 40 to 60 BPM.
- The HIS Bundle. This is an important part of the heart's electrical conduction system, as it transmits impulses from the AV node to the ventricles.
The heart nodes control this pumping action and allow for the heart chambers to relax (fill) and contract (pump) blood to create the ACLS heart rhythms as illustrated below:
You can actually see the above behavior in an ECG strip.
ACLS ECG Rhythm Interpretation
Now, if we go back to the ECG tracing, each wave and dip represents a piece of the heart. We assign each wave and dip a letter to distinguish specific waves and dips in the ECG strip.
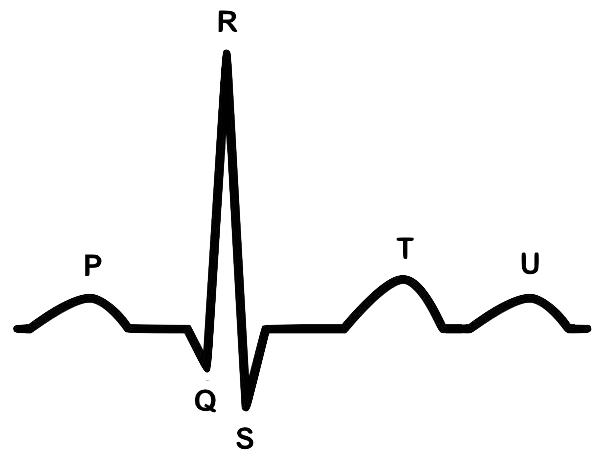
We decipher basic observations by reading the following components of the ACLS rhythm strip:
- The P wave: This represents a contraction of the atria. This is referred to as depolarization or the squeezing effect. This electrical wave in ACLS heart rhythms represents blood being pumped out of the atria and into the ventricles.
- The QRS Complex: This represents a contraction of the ventricles. This is the depolarization or squeezing of the ventricles. This entire wave complex represents blood being pumped out of the ventricles and into the rest of the body.
- The T Wave: This represents a relaxation of the ventricles. This is referred to as repolarization or filling of the ventricles. It represents blood filling the ventricles from the atria.
- The U Wave: This wave has no known reason for being there. So, we don’t have any normal interpretation. However, a prominent U-wave could indicate a serious cardiac issue.
During ACLS ECG rhythm interpretation, the ACLS heart rhythms show that the QRS complex stands out the most. This is because the ventricles in the heart are much bigger than the atria, indicating larger electrical activity.
Now, you may ask, why is there no wave indicating the atria repolarization? Well, you can’t see it on an ECG because the QRS complex is such a prominent electrical activity that it overtakes the relaxation wave of the Atria.
So now that we are equipped with knowledge of what each part of the ECG wave represents, we can utilize this information to identify arrhythmias and interpret algorithms according to ACLS AHA guidelines.
Common Heart Arrhythmias
Atrial Fibrillation (A-Fib)
Atrial fibrillation refers to a quiver, meaning an inadequate contraction. So whenever you hear A-Fib, you think of atrial quiver. A-Fib presents in the ACLS heart rhythms when the SA node is firing rapidly and creating an unusually high heart rate for the atria.
In basic terms, what’s happening is that the heart rate is so fast that the atria don’t have enough time or thrust to pump all the blood out of the atria and into the ventricles. This causes blood to stick around in the atria and circulate in the area for each heartbeat.
If you want to learn to read ACLS rhythm strips correctly, you must know that this is called stagnant blood, and we all know stagnant blood can eventually clot.
During the ACLS ECG rhythm interpretation, imagine the repercussions of blood clotting in the heart! If a blood clot travels from the atria and makes its way to the ventricles and then on to the lungs or anywhere else in the body, it could cause a pulmonary embolism or even a stroke if it travels to the brain. So, it's vital to recognize this early in ACLS heart rhythms to limit blood clots.
The animation below illustrates the atria giving off a faster-than-normal rate exhibited in A-Fib:
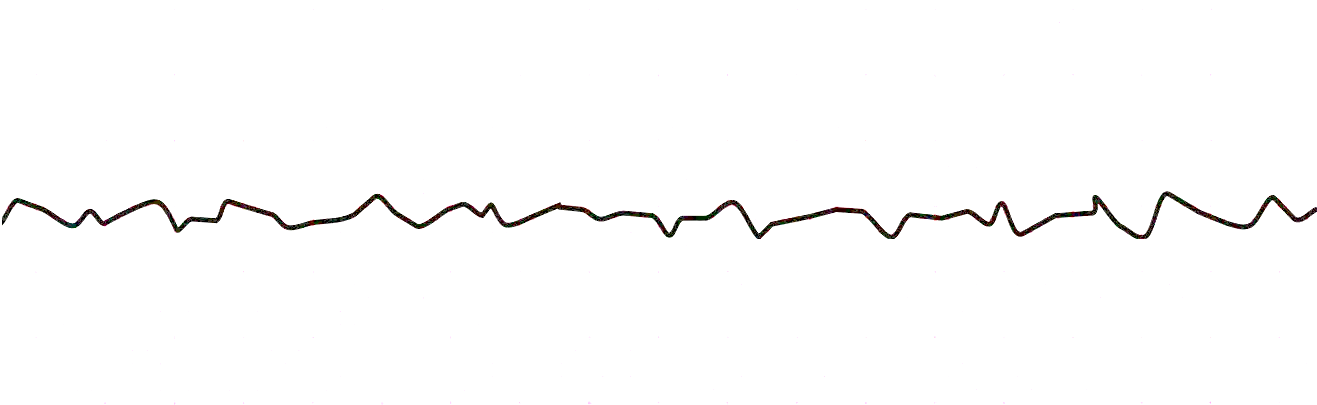
Here’s what the ECG rhythm looks like:
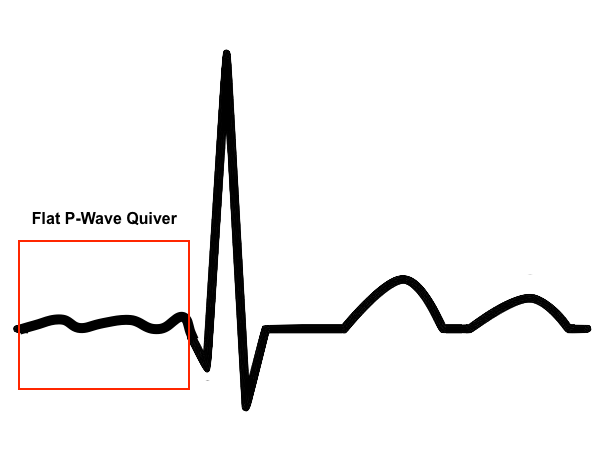
You can see the QRS complex that makes this rhythm unique (representing the ventricles). However, you can’t easily identify the P-Wave. It looks like a flat quiver. A-Fib is a very fast rate between 300 and 650 BPM. Patients exhibiting A-Fib symptoms are usually prescribed blood thinners to prevent blood clots from developing.
Atrial Flutter (A-Flutter)
A-Flutter is very similar to A-Fib in ACLS heart rhythms. It has the same rapid firing as the SA node, but usually not as fast. It usually is between 250-350 BPM.
The difference you will see during ACLS ECG rhythm interpretation in the ECG strip is that instead of the flat quiver for the P-wave, you see something referred to as a Saw Tooth. The P-wave looks like the teeth of a saw, with jagged lines.
However, as you can see, the QRS complex is still prominent and visible. Here’s what an Atrial Flutter ECG rhythm may look like:

Supra Ventricle Tachycardia (SVT)
SVT is also a very fast ACLS heart rhythm originating in the SA node. It’s usually exercise-induced and looks very similar to ventricular tachycardia but has an even faster heartbeat.
You can learn how to read ACLS rhythm strips and identify all the normal waves, but they are happening so fast that the waves seem to be compacted into each other.
The rate is usually around 100-300 BPM and can be reversed by performing vagal maneuvers (bearing down or ice packs, blowing through straw, etc). This can help trigger the SA node to kick back into normal ACLS heart rhythm. If not, you will have to move on to various medical therapies.
Here’s what a Supra Ventricle Tachycardia ECG rhythm may look like while you’re interpreting an ACLS ECG rhythm:
Ventricular Fibrillation (V-Fib)
V-Fib, just like A-Fib, refers to a quiver or inadequate contraction. However, this time, the quivering occurs in the ventricles.
This is a very serious arrhythmia and can be deadly (It's also a shockable rhythm). If the ventricles are quivering, then the blood isn't fully emptying. As a result, blood is not adequately sent to the rest of the body as it should.
This decreased blood perfusion in ACLS heart rhythms could suffocate the body with a lack of oxygen delivery.
Since the ventricles are contracting so quickly with no regard to the atrium, you will see quivering of the QRS complex. Since the QRS is such a prominent wave, it's going to create an erratic ECG wave that can look something like this:
Ventricular Tachycardia (V-Tach)
V-Tach is an abnormally fast rate within the ventricles. The ventricles are contracting too quickly with no regard to the atria.
In this ACLS ECG rhythm interpretation, you will see a wide QRS complex and very fast ACLS heart rhythms. The Q-Waves have defined high peaks. It's not as erratic as Ventricular Fibrillation, but if not treated soon, it can lead to V-Fib.
Here's an animation illustrating V-Tach in the heart:
Here's what a V-Tach ECG may look like:
Conclusion
There are many more types of arrhythmias and ACLS heart rhythms to study.
However, this guide should lay the framework for ECG analysis, teaching you how to read ACLS rhythm strips and allowing you to have a solid understanding before taking your online ACLS course or getting your PALS recertification.
If you’re looking for affordable online certifications, ProMed can help! With our easy-to-use online platform, you can get certified in hours and get reminders for recertification.
View our courses and get certified today!
